Psoriasis
Psoriasis is a common skin disease that can involve a wide variety of symptoms which appear on the skin or in extracutaneous areas, at any age. The disease has both physical and psychological consequences: coping with other people staring and the impact on your own self-esteem can quickly become unbearable. This purpose of this information document is to answer all the questions you have about psoriasis, to challenge certain misconceptions and to help you live better with the disease daily.

What is psoriasis?
Psoriasis is a chronic, inflammatory disease that most often occurs on the skin: during a flare-up, the skin's appearance changes and it becomes covered with plaques. Depending on the type of psoriasis, plaques can be more or less widespread, completely red or covered with thick white layers of skin, known as scales. Psoriasis plaques cause great discomfort, the urge to scratch is often intense, and giving in to this need only aggravates a flare-up.
Psoriasis is also an extracutaneous disease and patients may experience joint pain before, at the same time as, or after the first plaques appear. Psoriatic arthritis affects all types of joint: the spine, knees, fingers, etc.
However, contrary to popular belief, psoriasis does not only occur in adults, it can also affect children, sometimes from a very early age. What’s more, psoriasis is not contagious, it is impossible to "catch" psoriasis by shaking a co-worker's hand, for example.
What causes psoriasis?
Some of the causes of psoriasis have been established, while others still remain a mystery. The most important thing is to understand what is happening in the skin. The microscopic mechanisms of psoriasis involve immune cells and skin cells. This process very quickly spirals out of control and leads to an inflammatory state which causes the plaques that can be seen and/or the pain the patient feels.
Psoriasis flare-ups are triggered or aggravated by a range of environmental factors:
- weather conditions,
- certain medications,
- alcohol and tobacco use,
- stress,
- skin damage,
- etc.
The onset of psoriasis is dependent on the presence of predisposition genes, which explains why cases in the same family are not uncommon. However, psoriasis is not directly inherited! We inherit the genes from our parents, which may or may not be expressed, early on or later in life, depending on certain environmental factors.

The symptoms of psoriasis
Dermatologists are very familiar with psoriasis, which is fairly easy to diagnose because of its often distinctive symptoms.
Plaque psoriasis, the most common form, is characterized by red, well-defined plaques covered in thick layers of whitish, dead skin called scales.
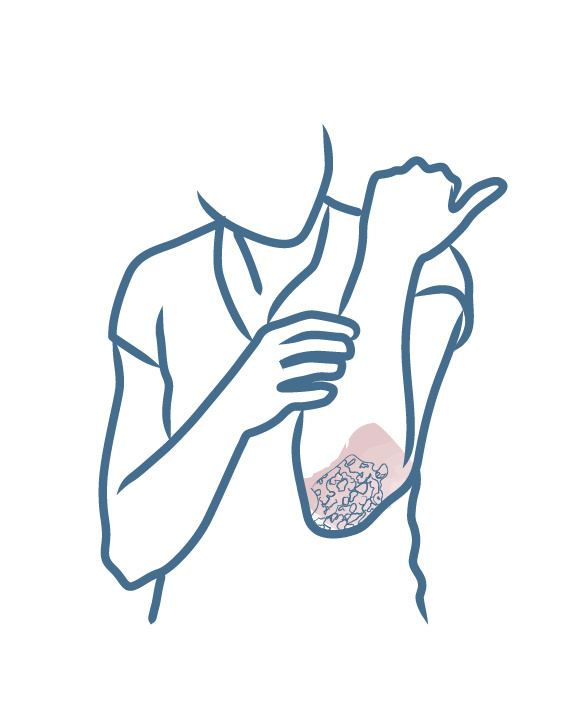
Psoriasis plaques can often cause intense itching which is difficult to ignore. Scratching removes the layer of scales, this leaves the red plaque unprotected and it may bleed. Scratching only slows down the healing process and prolongs the psoriasis flare-up. Ideally, you should let the scales become detached and fall off on their own, but no one wants flaky skin!
Outside of psoriasis flare-ups, skin is often dry, fragile and sensitive, and should be treated with the utmost care.
Diagnosis : you have plaques, dandruff, redness, itching ?
Do you have any of the following symptoms in your scalp and/or face and body?
- plaques
- dandruff
- redness
- itching
Wonder what it is?
It could be psoriasis, seborrheic dermatitis, or even eczema.
Make the diagnosis "Plaques, dandruff, redness and/or itching?" to discover our advice and recommendations for adapted care routines.

Areas affected by psoriasis
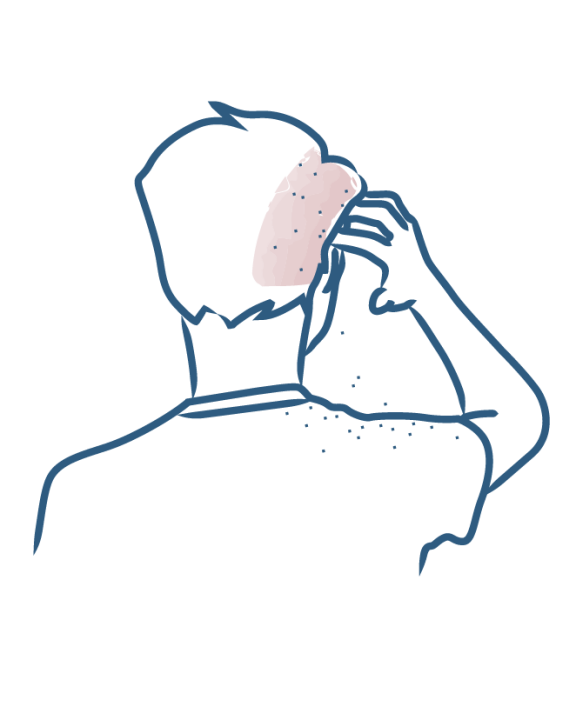
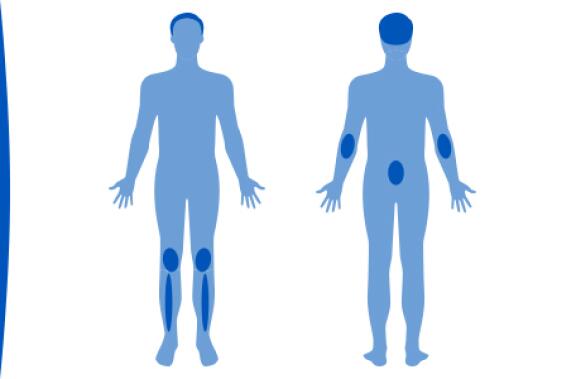
The locations where psoriasis can develop are extremely varied. Plaque psoriasis affects areas subject to friction such as the elbows, knees, legs and lower back. It is very common for the scalp to be affected.
But did you know that psoriasis can also affect the face, the nails, the palms of hands, the soles of feet and the genital area? There are as many forms of psoriasis as there are people affected. Each case is different and each part of the body affected is associated with different problems.
With scalp psoriasis, patients refrain from scratching in public to avoid attracting attention and to stop unsightly scales falling on to their shoulders; in cases of nail psoriasis, people often wear closed shoes and keep their hands in their pockets...
Psoriasis treatments
Psoriasis treatments are varied but they have one point in common: they are symptomatic treatments that reduce the symptoms of a flare-up but that do not prevent the development of a new flare-up. In other words, there is currently no definitive cure for psoriasis. Treatment is adapted to each person, according to their background, the history of their psoriasis, their needs and expectations.
Creams, especially those containing corticosteroids and vitamin D derivatives, are commonly prescribed as first-line treatment and may be sufficient if the psoriasis is not very widespread.
If creams are unsuccessful, other treatments may be prescribed to patients, such as oral treatments. Nowadays, the most severe cases are treated with injections known as biotherapies.
Phototherapy and hydrotherapy treatments are useful options for soothing psoriasis flare-ups. And research continues, with new treatments being developed every year!
Complementary therapies are increasingly popular. They can help people with psoriasis but should not be used as a substitute for basic treatments prescribed by a dermatologist.

Living daily with psoriasis
If you have psoriasis, you don't need to try and change everything about your life! Nevertheless, a few basic rules and some common sense can go a long way:
- it is essential to gently cleanse and care for your skin using suitable products
- eat a healthy and balanced diet
- avoid alcohol and smoking
- enjoy the sun's benefits but don't forget to apply sun protection.
- for the treatment prescribed by your dermatologist to be effective, it is important that you understand and follow it correctly
If you are struggling with the treatment or your psoriasis in general, speaking to friends or family members, caregivers or other patients can help you to externalize your anxiety and find solutions.
Our care routines
Psoriasis-prone skin
Dermatological expertise
To better understand your skin and hair, discover our exclusive content and innovative care products designed to improve your quality of life..